Treating Pain with Insight, Not Just Interventions
In a world of quick fixes, it’s time we asked a better question: what if healing chronic pain doesn’t start with medication, but with understanding?
The Problem with the Old Model
Since the age of bloodletting, we have treated pain like a mechanical problem. Pain was something to cut, scan, or drug away. But that model didn’t work with leeches, and it isn’t working today.
- In 2023 alone, over 80 million opioid prescriptions were written in the U.S., despite growing awareness of their risks.
- More than 130 Americans still die every day from opioid overdoses.
- Meanwhile, chronic pain remains the leading cause of long-term disability in America.
We’ve been masking pain, not managing it.
A Better Way Forward
Today’s best pain care looks radically different: it’s not just about tissues and tendons, but the whole person. It’s based on the biopsychosocial model, which considers biological injury and emotional, psychological, and social contributors.
“Pain that is understood is not to be feared. We can treat the nervous system therapeutically, not just pharmaceutically.” – Dr. Adriaan Louw
What This Looks Like in Action
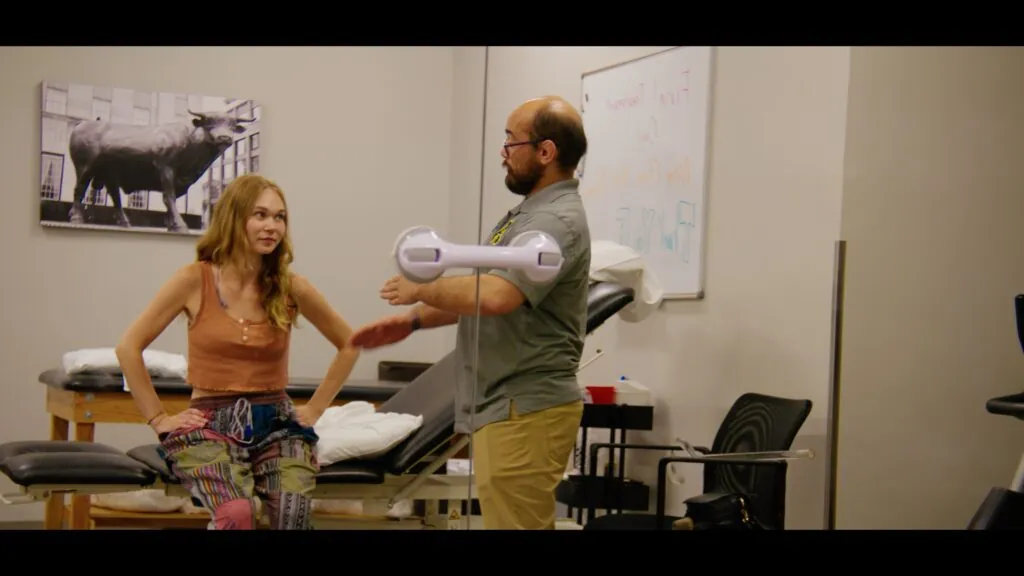
In Pain, Misunderstood, a short documentary exploring the chronic pain epidemic, we follow patients like Maddie, a young woman whose persistent pain wasn’t “in her head,” but deeply rooted in both her biology and lived experience. Her healing began when a PT finally listened and helped her understand what was happening in her body and why.
The Science Behind the Shift
Mindset changes biology. A Harvard study found that hotel workers who were told their daily tasks met exercise guidelines had significant health improvements – just from believing they were doing something good for their bodies.
PT can outperform psychology for pain. In a randomized controlled trial, physiotherapy that included stress inoculation and education was more effective in reducing pain and disability than exercise alone for whiplash-associated disorder.
Movement is medicine. Research out of Sweden found that 8 years of graded exercise significantly reduced inflammatory markers in people with rheumatoid arthritis, to the point where some no longer needed medication.
Why Rehab Professionals Matter
Physical therapists (PTs) and occupational therapists (OTs) are uniquely positioned to help patients recover, not just physically, but emotionally. They spend time with patients. They listen. They build trust.
“The healthcare system is transactional. But pain care has to be relational.”
— Dr. Stephen Clark, Chief Clinical Officer, Confluent Health
The goal? Not just less pain. But more function. More hope. More agency.
Who Needs to Hear This?
Anyone living with pain. Anyone treating it. Anyone who’s ever felt dismissed, labeled, or lost in the system.
Because all pain is real. And there is a better way.
“Enough is enough. More than 130 Americans will die today from prescription opioids.” – Adriaan Louw
References
- Sterling, M., et al. (2019). Physiotherapist-delivered stress inoculation training integrated with exercise versus physiotherapy exercise alone for acute whiplash-associated disorder (StressModex): a randomized controlled trial of a combined psychological/physical intervention. British Journal of Sports Medicine, 53(19), 1240–1247. https://doi.org/10.1136/bjsports-2018-100139
- Crum, A. J., & Langer, E. J. (2007). Mind-set matters: Exercise and the placebo effect. Psychological Science, 18(2), 165–171. https://doi.org/10.1111/j.1467-9280.2007.01867.x
- Löfgren, M., et al. (2018). Long-term effects of exercise on inflammation and health outcomes in patients with rheumatoid arthritis: A randomized controlled trial. Arthritis Research & Therapy. https://doi.org/10.1186/s13075-018-1758-x
- Louw, A. & Riera-Gilley, V. (2024). Pain Neuroscience Education: Teaching People About Pain. Journal of Pain & Palliative Care Pharmacotherapy. https://doi.org/10.1080/15360288.2024.2424853