- Home
- Conditions We Treat
- Sciatica/Nerve Pain
Sciatica refers to pain, weakness, numbness, or tingling that radiates along the sciatic nerve, which extends from the lower back through the hip and thigh. Depending on its severity, symptoms can also extend into the lower leg and foot. Sciatica can be caused by compression of the sciatic nerve close to the spine. Postural problems or poor body mechanics while sitting or standing at work can create tightness that impacts the sciatic nerve. Our physical therapists create personalized treatment plans as each patient’s pain differs. Some modalities your physical therapist may use include:
Stretches for sciatica aim to improve the mobility of the nerve and reduce symptoms of compression.
Sciatica describes the symptoms of an underlying medical condition, indicating irritation or injury to the sciatic nerve. It is a relatively common condition that affects up to 40% of people over their lifetime.1 The highest incidence occurs between the ages of 30 and 50. Generally, people under 40 experience sciatica due to a herniated disc, while the cause for adults over 40 is usually related to arthritis or general wear and tear on the spine.
Sciatic nerve pain can be debilitating. Symptoms can significantly impact quality of life, hindering the ability to perform daily and job-related tasks.
Sciatica can occur when there is irritation or injury to the sciatic nerve. Several underlying conditions may contribute to sciatica. Common causes include:
Low back irritation can occur when there is injury to muscles and other soft tissues of the low back. This irritation can lead to compression or chemical irritation of the sciatic nerve, which may cause sciatica symptoms.
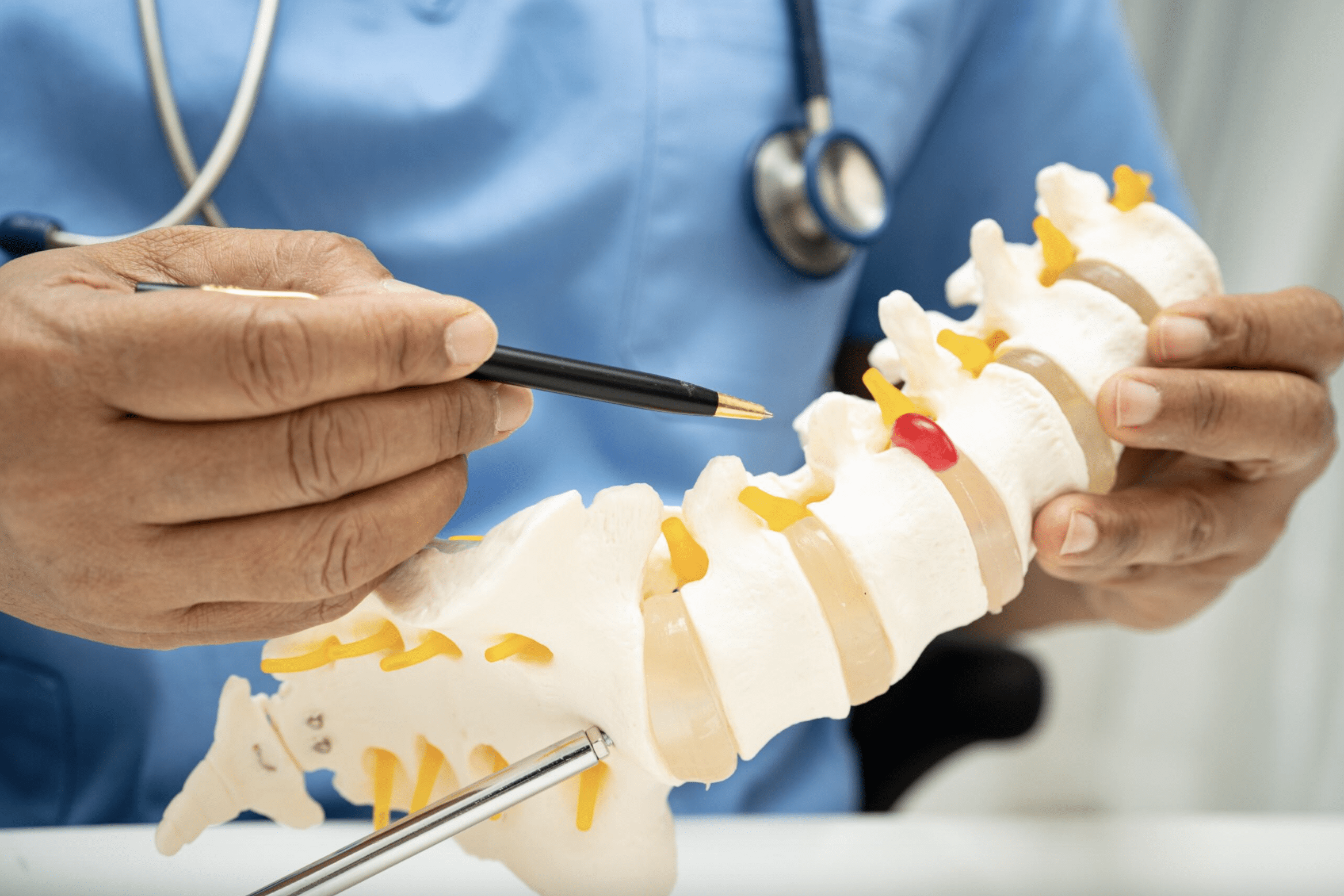
A herniated disk occurs when the soft tissue between the spinal bones (vertebrae) protrudes and presses on the sciatic nerve. This soft tissue, called a spinal disk, is used as cushioning between the vertebrae. It is more likely to occur with age, although it can also result from an injury to the spine.
Spinal stenosis occurs when the space inside the spine becomes too narrow, putting pressure on the spinal cord and nerve roots. This narrowing typically happens due to natural wear and tear on the spine during aging. When this occurs at the sciatic nerve root, it can cause irritation, leading to sciatica pain.
Degenerative disk disease occurs when the spinal disks wear away due to natural wear and tear on the spine with age. As the disks lose height, the bones of the spine get closer and can rub together. This can lead to herniated disks, spinal stenosis, or spondylolisthesis, a condition in which the vertebrae move out of alignment. Any of these conditions can irritate the nerves of the spine, potentially leading to sciatica.
Spondylolisthesis happens when one of the vertebrae moves out of alignment. This can occur due to natural wear and tear on the spine, growth spurts, or injury. The misalignment can put pressure on the nerves of the spine, potentially causing irritation to the sciatic nerve root.
Several risk factors are associated with sciatica, including age, obesity, and occupation. Luckily, most of these risk factors can be changed with intervention. The primary non-modifiable risk factor is age, with sciatica occurring more frequently in those aged 30–50.
Modifiable risk factors include smoking, obesity, physical inactivity, prolonged standing or sitting, and frequent heavy lifting. While some occupational risk factors may be challenging to adjust, making changes toward a healthier lifestyle is recommended to reduce the risk of sciatica.

Common sciatica symptoms include pain, numbness, tingling, and potentially muscle weakness. It may also feel like a muscle cramp that will not go away. The pain can occur anywhere from the lower back to the toes. Many describe it as sharp, shooting, or burning, similar to an electric shock. The pain may worsen with specific movements, such as twisting, coughing, or sneezing, or certain positions, like prolonged sitting.
Numbness can occur along the lower back or affected leg, leading to decreased sensation on the skin in those areas. This happens when the irritation or injury caused by the underlying condition disrupts the sciatic nerve signal. Tingling, or paraesthesia, is the sensation of pins and needles on the skin of the affected leg. It can also be described as a prickling or itchy feeling. Pressure or irritation to the sciatic nerve may also cause this symptom.
In more severe cases, muscle weakness or incontinence issues may occur. Worsening muscle weakness, difficulty with bladder or bowel movements, and fever accompanying back pain are red flag symptoms. These may indicate a serious underlying condition and warrant a referral to a medical doctor.
Talk to a physical therapist if you experience moderate or worsening pain, numbness, or tingling in your lower back, hip, or leg.
Your physical therapist will perform a detailed evaluation during your first visit. In addition to taking a comprehensive medical history, your physical therapist will ask questions about your pain, including duration, severity, and characteristics. They will also perform various physical tests to assess your range of motion, strength, and muscle tenderness. Using this information, they will determine the best course of treatment for your specific case.

Physical therapy is a commonly prescribed conservative sciatica treatment. It is effective at reducing pain intensity and disability, especially when prescribed early in the course of treatment.2 Many people will display “directional preference,” a clinical phenomenon where a specific movement can provide relief from pain and symptoms. Typically, a person will fall into one of two categories:
Correspondingly, you may display an intolerance toward specific movements:
Once your physical therapist determines your preference, this movement can be repeated or held to improve symptoms.
Your physical therapist will develop a treatment plan based on your individual needs. This treatment plan will initially focus on minimizing time in positions of intolerance while encouraging movement in your directional preference. Gradually, your physical therapist will help you reintroduce positions of intolerance to improve function and overall quality of life.
While working with your directional preference, you will also perform exercises to maintain and improve general strength and mobility. These exercises usually focus on the lower back, hips, and legs. Your physical therapist will help determine which exercises work best for you.
Sometimes, your PT may refer you to a medical doctor for adjunct treatment to help facilitate rehabilitation or if you hit a plateau. Your doctor may then advise using medications to relieve sciatica pain. These medications could include over-the-counter pain relievers like NSAIDs or prescription medications like corticosteroids or muscle relaxants. Be sure to speak with your doctor before taking any medication.
Surgery may be an option when conservative treatments fail. There are many reasons surgery may be recommended, including worsening neurological symptoms or severe effects on quality of life. The decision to undergo surgery should not be taken lightly—failure rates have been estimated between 10% and 40%3.
Standard surgical procedures include microdiscectomy, laminectomy, spinal fusion, or artificial disc replacement. Microdiscectomies and laminectomies are procedures that remove part of the spinal disk or spinal bone around the affected area. Spinal fusions permanently join two or more vertebrae to stabilize the area around an irritated nerve. Artificial disk replacements replace a damaged spinal disk with a synthetic replica. All the procedures are intended to reduce pressure and irritation on the sciatic nerve to relieve pain.

Physical activity is one of the best ways to reduce your sciatica risk.4 Set a timer and take a short walk every hour, or use your lunchtime to get some steps in. Do what you can to limit sitting time and move as much as you can during the day.
Physical activity is an excellent way to reduce the risk of sciatica. In addition to light cardio activity, like walking, you can also perform a variety of exercises. Your physical therapist will help determine the best exercises for your specific case. However, there are general options that can be beneficial as well.
Certain lower back and hip stretches can help. This may improve overall function and increase your quality of life.5 Graded exposure to strengthening exercises is important. Start with movements that do not cause pain, then progress to more advanced movements. Talk to your physical therapist for individualized exercise recommendations that work for your lifestyle.
As mentioned above, staying physically active is one of the best ways to prevent sciatica. Engage in moderate-intensity exercise as often as possible to keep your body strong and flexible.
Smoking cessation is a must for reducing your risk of sciatica. Smoking can damage the circulatory and nervous systems, so quitting smoking can be beneficial in preventing issues in these systems.
Stress management is critical for many reasons, including reducing the risk of sciatica. Use self-care strategies such as exercise, nutritious food, and sleep hygiene to manage daily stress. Meditation, deep breathing techniques, or yoga may also help control stress levels. Maintaining a healthy weight may also help reduce your risk of sciatica.6
Dealing with sciatica pain requires a multipart treatment strategy. Physical therapy can help reduce pain and symptoms. Pain-relieving medications and modalities, such as heat and ice, can also help manage symptoms. In addition, maintaining a regular sleep schedule and striving for a healthy lifestyle are excellent ways to cope with pain.
If you experience a flare-up, try to identify the triggering factors to avoid them in the future. As soon as possible, utilize pain-relieving techniques such as heat, ice, or medications. Perform your prescribed exercise routine within your ability. If your pain persists or worsens, contact your physical therapist.
When you book an evaluation with Confluent Health, your physical therapist will guide you through a treatment plan tailored to your unique needs. From individualized exercise programs to skilled manual therapy techniques, our goal is to help you feel better and get back to your life.
One foundation of a successful treatment plan is patient education. Our physical therapists are experts in providing easy-to-understand education that applies to your situation. They will ensure you are comfortable with every aspect of your care, including home exercise programs and workplace ergonomic recommendations.
Confluent Health can also help you return to sport or work with confidence. Our sport-specific rehabilitation programs are designed to help you return to the game you love, while our work conditioning programs will help you regain strength and function so that you can return to work.
You should follow your physical therapist’s recommendations. Typically, they will prescribe daily exercises specific to your condition.
Yes, light exercise is often beneficial in reducing sciatica symptoms. Ensure you are exercising within your ability, and stop if symptoms worsen. Consult a healthcare professional for more specific, tailored guidance.
Most likely not. The majority of cases respond well to conservative treatment. Surgery is only necessary for severe cases or when conservative treatment fails.
Resources